Simulation to create specific surgical technical skills even when operating space and patient size are limited
Pediatric surgical training has undergone many changes over the last decade and, as with many surgical branches, it is becoming increasingly difficult to ensure adequate training for physicians in specialized training.
In pediatric surgery we treat many malformations and diseases, some even rare, that require the acquisition of specific skills for each of them. It is difficult for a student to obtain adequate experience in medium and large surgeries by attending a single center. Other factors also aggravate the situation: on the one hand, the acceleration of the transition from the world of training to the labor market, with people in training hired to fill positions when they have not yet completed the training cycle; on the other hand, the decrease in births, not only due to demographic decline, but also in association with more accurate prenatal diagnoses that lead to early termination of pregnancy in complex malformation cases; finally, the lack of specificity in the pediatric surgical sector, which leads the community to ignore the existence of specialist surgeons trained in child care, and unfortunately about 25% of children who need surgery are cared for by adult specialists in non-pediatric rooms. All this for the pediatric surgeon, in training or not, translates into a reduction in the number of cases to operate.
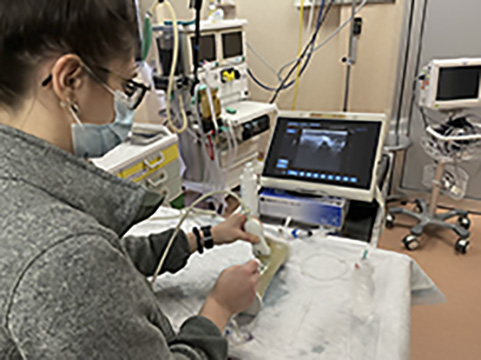
As with other surgical specialties, to ensure the correct training of the pediatric surgeon, the development of simulation systems capable of creating specific surgical technical skills is essential. A challenge according to the times that contains within itself another challenge. Because it is not only necessary to ensure the highest level of quality in the correction of any malformation condition, offering general and specific training for each pathology and for each child. The peculiarities of the pediatric patient must also be taken into account: the pediatric surgeon treats patients with a very wide age range, from 0 to 18 years of age, with completely different physical characteristics in morphometric terms. If we then talk about minimally invasive techniques such as laparoscopic, thoracoscopic and robotic surgery, the small anatomical structures of children and the limited space of the cavities represent one of the most critical issues to address: surgically treating a defect in a 10-month-old baby Compared to a 17-year-old, although the anatomy is almost similar, it looks completely different, as the space to operate on and the size of the anatomical structures involved vary greatly.
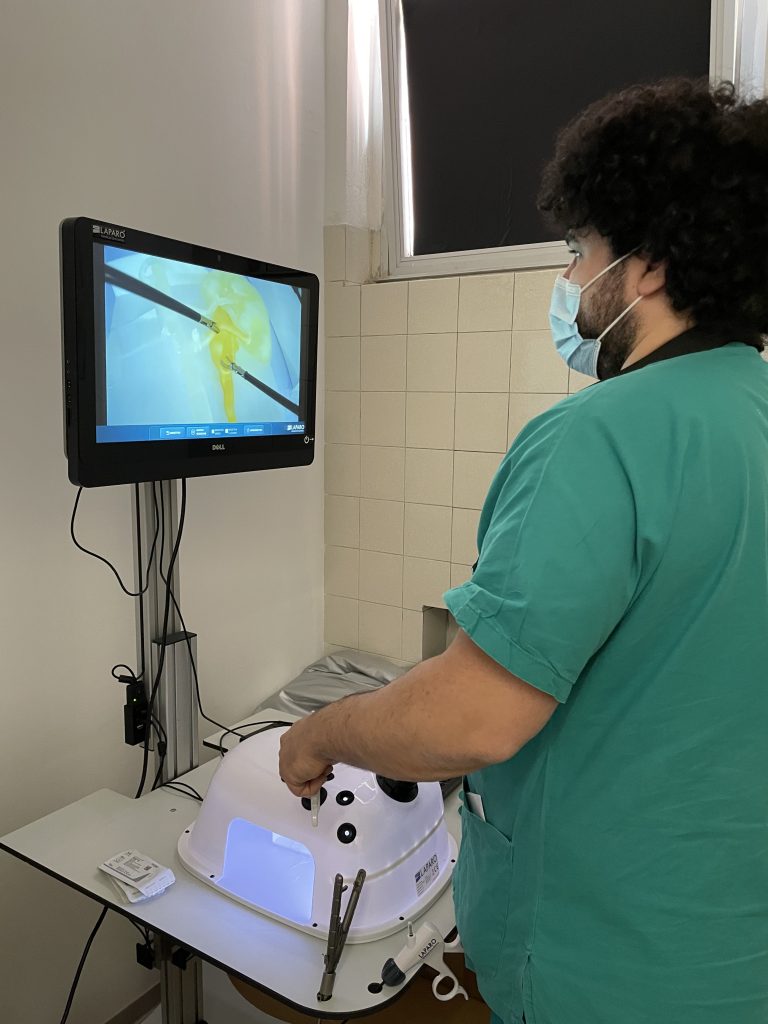
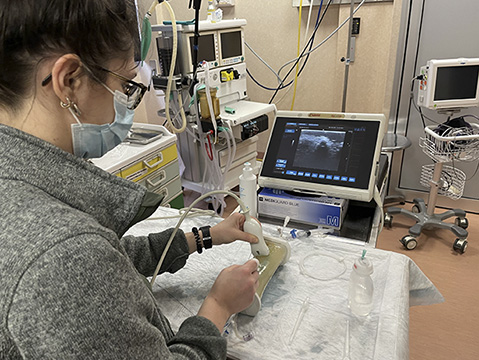
From this need arises useful and current, to develop simulators that combine the advantages of the various types of simulation models such as physical and virtual ones – including realism, procedure repeatability and low cost – that allow improving the learning curves of the young pediatric surgeons in limited space settings. Virtual simulation certainly represents a possibility, with modern computer technologies making it possible to develop convincing representations of an apparatus or body region, with interaction possibilities including manipulation, dissection, and suturing. But despite the inexhaustible number of exercises that they allow, the absence of tactile feedback and, above all, the impossibility of reproducing spatial triangulations limited by size represent a limit to their use. Therefore, it is essential to be able to develop physical simulation models, using materials that realistically reproduce individual anatomical districts, faithfully representing the reduced dimensions and allowing to recreate an entire procedure or a single skill required during its use.

However, creating models that have a high degree of realism in the pediatric field is not easy: functional structures for the purpose must be identified, materials must be carefully chosen, specific skills in the reproduction of small structures must be developed, and, above all, it is necessary to have the time to carry out the tests and for the model to be tested by experienced surgeons, to have feedback and try to reach the optimum level of quality.
By merging 3D printing and simulation techniques, it is possible to achieve this goal by recreating patient-specific models, at low cost and in a short time, from three-dimensional radiological images (MRI and CT). But to do this, proper structures are needed, such as dedicated print labs, along with qualified engineering staff flanked by expert pediatric surgeons who know the critical issues that will be reproduced in each model.
The challenge of the new decade has just begun, but the prospects in this regard are excellent, with a double advantage: on the one hand, the possibility of changing the training of the pediatric surgeon of the future, and on the other hand, helping even expert surgeons to maintain the skills acquired through simulation before performing less frequent surgical procedures, as well as giving them the opportunity to become practical with new minimally invasive techniques.
READ ALSO