Juanjo Zafra tells us about MegaEcode, a training project for physicians using simulation and ultrasound in CPR maneuvers, aimed at attendings and residents. This innovative program seeks to improve standards of care and diagnostic efficiency, using resources such as ultrasound scanners and alternative didactic methods for more effective and realistic medical education.
I am Juanjo Zafra, a hospital emergency physician in the Osakidetza (Basque Health Service) network in northern Spain, and I speak on behalf of three physicians who have embarked on a special teaching adventure.
We belong to the emergency department of the regional hospital San Eloy, in the integrated health organization OSI Barakaldo-Sestao, which has approximately 21 doctors and 12 residents (doctors in training) of the 4 years of the specialty Family and Community Medicine.

What has been our training proposal?
Together with two other emergency medical colleagues, Ana Lourdes Iglesias and Elena Gregorio, I embarked a year ago on a project (with a system such as simulation, not used until then in our work environment), which we call MegaEcode, based on the need that we professionals have for training and recycling in all techniques and maneuvers of daily use to maintain a standard of medical care, including resuscitation. In order to improve the management and consequent results supported by new diagnostic tools for use by emergency physicians, we integrate ultrasound in the usual maneuvers in CPR to achieve greater efficiency and more optimal results.
Who is our target audience?
We focused our target audience on both attendings and residents, all in a simulation environment, moving away from the typical teacher/student static training.
What did we need?
For this we needed something that we already had covered: the teaching staff and the subsequent support of the head and direction/management of our OSI (from here our deepest thanks).
We believed that the teaching staff was adequate for the organization of this training: a medical colleague accredited as an instructor by the American Heart Association (AHA), another medical colleague with extensive teaching experience and a medical technofriki coordinator of the working group of ultrasound by the Spanish society of emergency medicine and emergency of Euskadi (SEMES-EKALME), all of them tutors of residents.
We created different cases to perform the simulation with the use of ultrasound, application of CPR protocols replicating on screen our patient management program (Osabide) generating fictitious patients and adding videos of other professionals to whom interconsultations could be performed, embedded in a Powerpoint that integrated everything.
The support of the management meant that we were able to free up shifts to dedicate ourselves to this project and, together with the direction and management, we could count on the hardware, devices, location and other infrastructures.

How did we start?
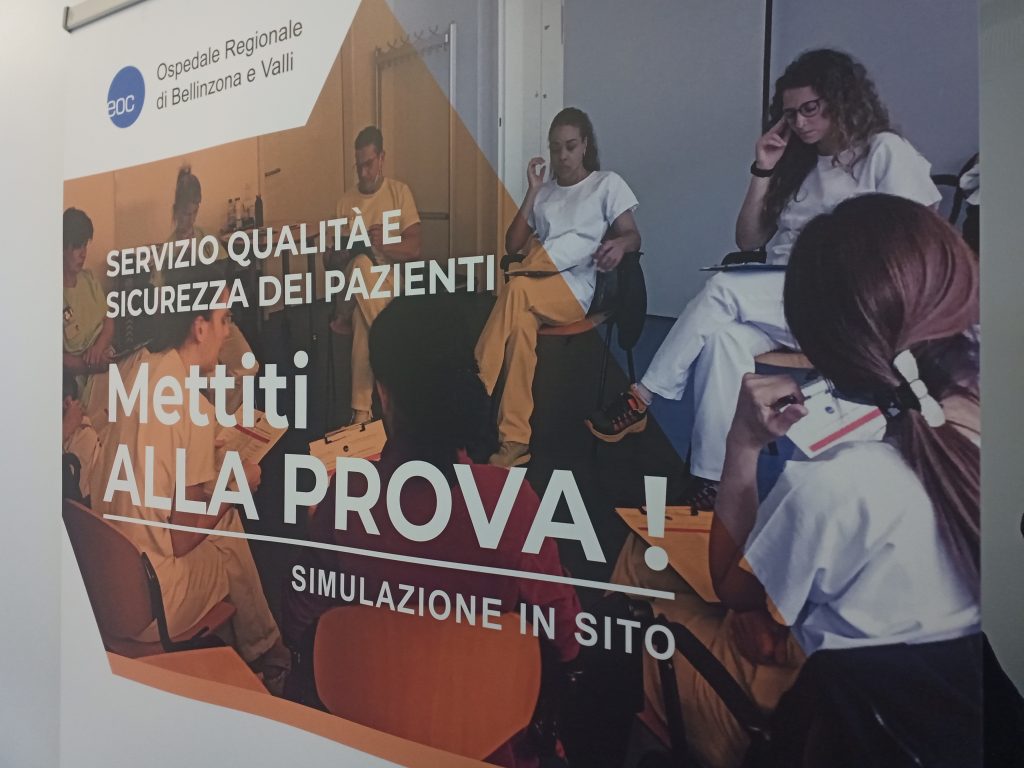
Initially and with pilot groups of residents, we started in the hospital’s meeting room, which we set up as an ICU (with all the differences you can imagine) with a manikin previously used in CPR training, with one of the ultrasound scanners in the emergency room and with iSimulate simulation devices with which we exposed the rhythms, analytical and ultrasound scans. The most curious thing was the CT scan we used, which we performed with cork and floating pool tubes, recording the entire simulation with our own cell phones and tablets.
We saw that the main thing about the simulation was the desire, the passion with which we approached the planning of the case. Everything else (fiction engagement, debriefing…) which is also necessary, as we saw later in our own training as instructors (training that we consider indispensable and which we will talk about later) would come as a matter of course.
After the first simulations in the hospital, we “conquered” a prefabricated module with several rooms dedicated to vaccination and Covid management (diagnostic tests, vaccines…), adapting two of these rooms, always with the awareness of going step by step.
How did we optimize resources?
As I say, we went step by step, first informing ourselves of what was necessary, requesting from our management what we thought was indispensable, such as a Gesell camera (that one-way mirror that prevents being seen from the simulation room), room decoration with vinyl to give more realism and looking for economic alternatives to improve.
It was not a matter of “going “all out of the window” but to surround ourselves with material that would be useful for our objective. We already had the iSimulate devices and the ultrasound scanner shared by the emergency department. We expanded the family with an intubable manikin torso. And the next step was to
optimize, taking advantage of existing computer terminals, expired and/or discarded medical material such as intubation material, respirator…, and efficiently searching, in different web platforms, for the necessary devices.
We discarded high resolution cameras from companies that supplied our healthcare organization, opting to acquire, through platforms such as Amazon, web cameras with audio that we improved with the purchase of bluetooth microphones. We used our own cell phones for communication with confederates (doctors infiltrated on stage) and speakers for distant siren sounds, etc.

How did we train?
We realized that in order to speak properly and do things right we needed training. We attended a course for simulation instructors at the Francisco Vitoria University in Madrid (a salute to all the trainers from whom we learned a lot) and after some further work we managed to acquire the skills to become simulation instructors.
As we could see the simulation had nuances that we did not cover and our initial good work insisted on concepts that we had to reduce weight.
What is our current situation?
Now we are giving the second teaching round to both attendings and residents, already speaking properly (humbly said) from the point of view of trained instructors and with our newly purchased slate to make better debriefings, collecting surveys with a very good evaluation.
We want to extend the training to other professionals, other specialists, anyone who requests it.
Soon we will start the simulation with continuous care personnel (PAC) and we continue with the same or even more enthusiasm and passion. We make our project visible in several congresses and conferences (highlighting the Conference of Recognition of Good Practices of Osakidetza held at Cruces Hospital and the VII National Congress of the Spanish Society of Specialized Health Training and XIX Meeting of Tutors and Heads of Study in Santander) as well as in specialized magazines such as the one you are reading.

Anything else to add?
Yes, the basics. We consider simulation to be indispensable for dealing with situations in controlled environments; situations whose management may be compromised by the low incidence depending on the setting.
And with this, we underline that the important thing for any project is the illusion that is put into an idea.
Everything else will come on its own. Or we will simulate it.
READ ALSO