Simulated or standardized patient: 10 tips to get the most out of it
The simulated or “standardized” patient is an important simulation modality for the training and evaluation of students. This is a qualified individual who is able to simulate all aspects of a real patient with the goal of having students practice in various clinical scenarios to gain skills and confidence, make mistakes and receive valuable feedback for improvement before treating real patients. In addition to portraying an illness, the simulated patient is trained to provide constructive feedback to students so that they can develop their professional persona with the help of the patient’s point of view. Here are 10 practical tips for building a learning station using this simulation mode.
1. Decide if the patient is simulated or standardized
The situations of use, the environment and the objectives of the training determine the difference between “simulated patient” and “standardized patient”. The simulated patient, respecting the script, within the simulation scenario for training purposes, can represent their own characteristics (for example: more or less talkative, more or less aggressive, etc.). When the goal of the scenario is assessment, the patient is “standardized” in that it must always represent the patient’s characteristics in the same way to ensure an equitable experience for all learners.
2. Set training goals and key actions
Specifically identify the general objective (eg, perform an anamnestic compilation), specific objectives (eg, collect family history, medication history, etc.), and indicate the key actions (eg, perform physical examination, use validated evaluation tools, etc.).
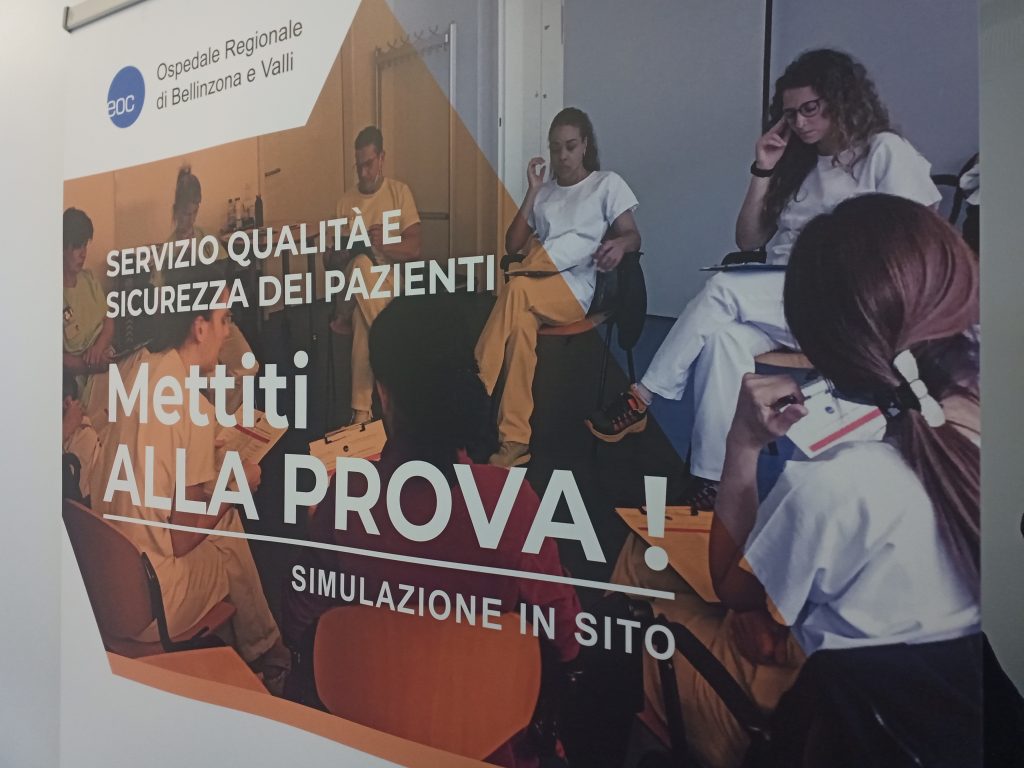
3. Recreate a situation as likely as possible
Recreate the situation from reality (for example, a frequent event for which an approach must be standardized, or the management of particular communication-relational problems, etc.), taking care of the scenario also in terms of setting and moulage to enhance the immersive experience. Simulation in a protected environment is safe for students and improves patient safety.
4. Write the script.
There are several types of templates. Choose the one that best suits your needs. Remember to ALWAYS include: (a) the actions/behaviors of the actor, (b) the psychological profile, (c) the emotional state, (d) the information that will be freely provided during the simulation, (e) the information that will be provided ONLY if the student requests it and (f) the information that will be given ONLY after certain actions are performed by the student; (g) any moulage to be performed, (h) additional materials needed, (i) appropriate spaces. Based on the script, the choice of the right actor to play that role will be determined.
5. Send the script to the SP and schedule the simulated patient training.
The script must be sent to the actor well in advance, especially if they are volunteer actors who guarantee availability in their free time. We will work together to better represent the expected role, paying special attention to the training objectives and the clinical condition to be represented. Watching explanatory videos can be helpful.
6. Test the scenario
Test the scenario, even multiple times. This is necessary to make any change, even under suggestion of the simulated patient, also to the representation of the affective-relational aspect that is to be recreated.
7. Set Simulated Patient Feedback After Simulation
During the training it is important that the simulated patient, with the help of the trainer, learns to give feedback to the trainee, focusing the reference on their experience as a patient and on the specific actions carried out by the trainees during the scenario.
8. Rehearse the debriefing of the scenario with the participation of the simulated patient
During the training, in addition to the scenario, also try the debriefing, leaving adequate space for feedback from the simulated patient, who should participate immediately after the students who acted out the scenario. The scenario with the simulated patient is in effect a didactic tool and produces its effects thanks to the guided reflection during the debriefing. The use of video recording can be useful to review what happened in the simulation and stimulate discussion and critical reflection.
9. Make sure participants are familiar with the simulation mechanism of the simulated patient
Clarify what is expected from the simulated patient, what can be done (eg, auscultation of heart tones, etc.), what items instructors will provide (eg, altered vital parameters), and what must be done in the task trainer.
10. Schedule a final analysis
Do not forget to take time at the end of all training to perform a reverse analysis and verify the achievement of the objectives and reflect, together with the simulated patient, on the critical points that have arisen.
READ ALSO