This time Athena Ryals explores the challenges of achieving fidelity in simulation within medical education, highlighting the discomfort students face when navigating simulated scenarios. Despite the use of high-fidelity tools and realistic settings, learners often struggle due to the absence of familiar social rules. Athena, a Simulation Operations Specialist, suggests that this discomfort may stem from the fact that simulation exists in a structure outside of the regular world, which favors neurotypical individuals. And she invites further discussion on how to better prepare students for simulations, considering neurodiversity and the inherent societal biases in medical training.
“Are we supposed to touch the manikin, or do we just say what we would do?”
“Are you playing the nurse right now, or our teacher?”
“Should we actually give the medication?”
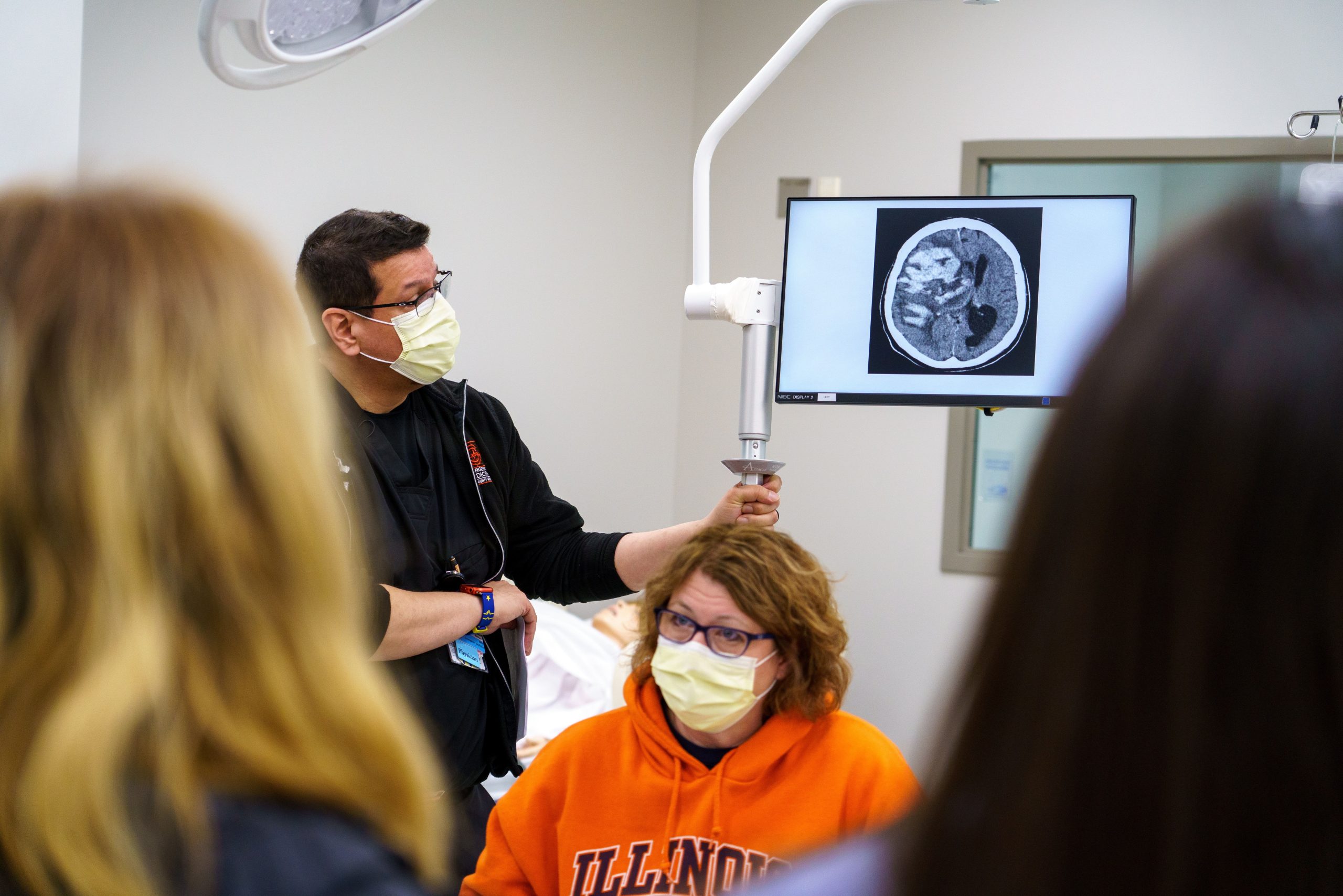
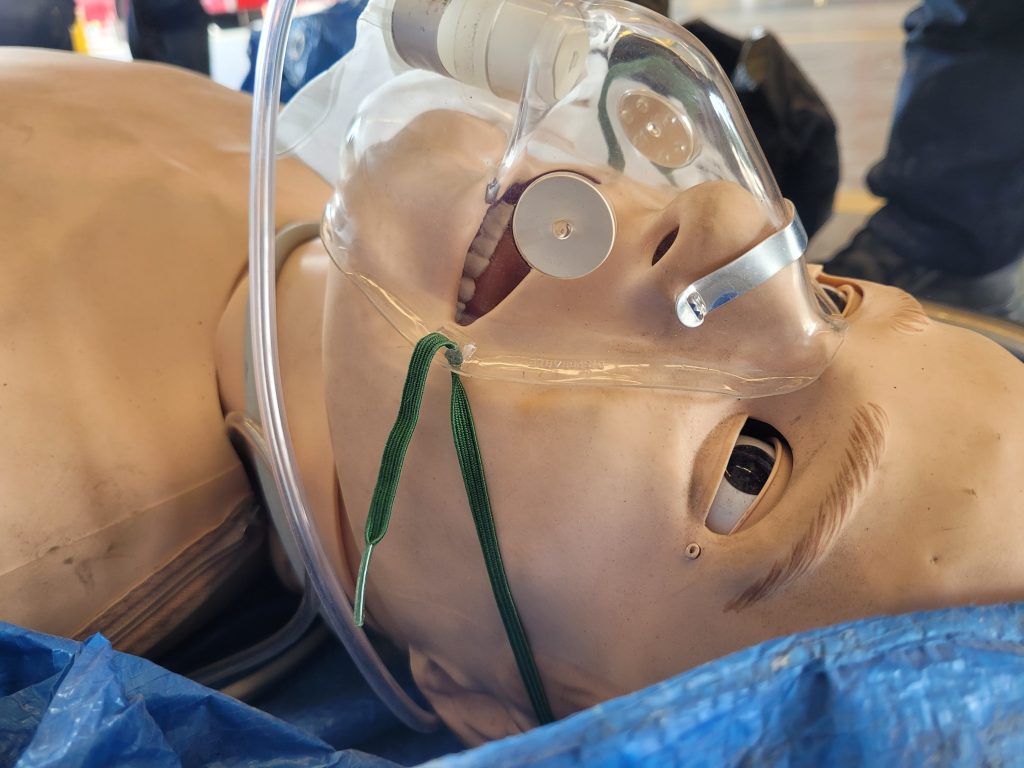
These are questions I hear almost every time I run a simulation as a Simulation Operations Specialist. My simulation center primarily serves undergraduate medical students in the first year or so of their education. Students nervously shuffle into the room and huddle together even though we wish they would step forward and take command of the situation. We use every tool in our toolkit in order to make the simulation as fidelitous as possible: a real, operating headboard with dials so you can administer oxygen (it’s just compressed gas, but the students don’t have to know that) medication boxes from Demo Dose that we painstakingly refill with distilled water after every session, and an expensive manikin as the centerpiece that costs more than I make in a year – by a lot. And still, without fail, no matter how good my moulage is or how dedicated our Standardized Patient is or how attuned our facilitator is to the flow of the scenario, the students still seem paralyzed with questions of how to navigate this situation that we as Simulation Professionals try our best to make straightforward.
This isn’t simply a gripe I have about my job, though, and I don’t want to sound like I’m complaining about my students. Fidelity, realism, and learner immersion are hot topics in the world of simulation at the moment. Simulationists push for higher and higher fidelity through expensive simulators and XR in the hopes that higher fidelity equals better learning outcomes – although the data suggests that learning outcomes remain the same whether the simulation is conducted with high fidelity or low fidelity 1,2,3. It can therefore be frustrating when we are doing everything humanly possible to make the simulation real and engaging, and our students still walk into it questioning the basic rules of the interaction.
Allow me to suggest a different perspective.
These behaviors, to me, look like my internal monologue during almost every social interaction. And I am neurodivergent.
I see these students outside of simulations, and they act entirely differently. They may be shy, brash, contemplative, or whatever their personality or the situation may call for, but they do in some way occupy their space without outwardly questioning how they should be doing it. Society has a structure, and they know the rules. They play by them. They adhere to them.
However, as soon as they step into a simulation, the rules are unknown, and that is crushingly uncomfortable. I would posit a guess that this is the reason why it is so difficult to get learners in the door, even if they have been practicing medicine for years and by all rights should breeze through a simulation with ease. Test anxiety may have a lot to do with it, yes. Nervousness at the idea of being scrutinized may have something to do with it, too. But allow me to suggest that a large reason why most people find being in a simulation so off-putting is that for the duration of the simulation, they are outside the rules and structure of the “normal” world, and they find that deeply unsettling.
I think this effect is further exacerbated by the fact that medicine specifically selects for neurotypical people – people who naturally, intuitively pick up on and adhere to the invisible structures created and enforced by society. Only about 4% of physicians in the United States report having a disability. 4 (There is another conversation to be had about neurodiversity being a disability versus a neurotype versus an identity, but that is a conversation for another time.) Only about 3% of physicians in the UK identify as autistic. 5 And when neurodivergent clinicians are talked about in medicine, they are talked about as “assets”5 and having “untapped potential”6 – the way you would talk about a car or a fixer-upper house, not a human being. Medicine selects for neurotypical people in many ways, and neurotypical people are used to knowing the rules of engagement.
Therefore, if a neurotypical learner – who all their life has been able to navigate the pitfalls and snags of conversation, the unsaid taboos and generally understood rituals of interaction that, to me, feel completely arbitrary – enters a simulation where those rules may no longer apply, then it makes sense that the loss of that structure would feel extremely disturbing. It’s no wonder we hold entire conferences and courses on how to get people into simulation. We’re asking them to abandon the very structure that makes them feel safe, every time we do!
What is the solution for this? I’m not sure I have one. It’s possible that we could tackle this issue with more rigorous prebriefs, going over the use of every manikin, embedded participant, and piece of equipment. However, this does not seem like the answer. To me, the issue of simulation fidelity feels tied to these large concepts of society and structural bias and neurodivergence, which would explain the struggles we as an industry have had in increasing learner buy-in with fidelity. I invite other perspectives on this. I have simply noticed what seems like a connection, and I’m wondering if my peers have further insights or even solutions.
Until then, I think we’re going to have to keep assuring our students of the rules of the simulation, no matter how fidelitous we make it. After all, by the very definition of simulation, it is not real life. Therefore, navigating the unseen snags of the scenario may remain a terrifying unknown to our students for as long as society, simulation, and neurotypicality itself, exists.
References:
- Weyers, A. R., von Waldenfels, G., Gebert, P., Henrich, W., & Hinkson, L. (2024). Reducing trainee mistakes. better performance with changing to a high-fidelity simulation system? AJOG Global Reports, 4(2), 100326. https://doi.org/10.1016/j.xagr.2024.100326
- Lejus-Bourdeau, C., Pousset, F., Magne, C., Bazin, O., Grillot, N., & Pichenot, V. (2023). Low-cost versus high-fidelity pediatric simulators for difficult airway management training: A randomized study in continuing medical education. Brazilian Journal of Anesthesiology (English Edition), 73(3), 250–257. https://doi.org/10.1016/j.bjane.2021.05.006
- Mitchell, S., Blanchard, E., Curran, V., Hoadley, T., Donoghue, A., & Lockey, A. (2024). Effects of simulation fidelity on health care providers on Team Training—a systematic review. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 19(1S). https://doi.org/10.1097/sih.0000000000000762
- Nouri, Z., Dill, M. J., Conrad, S. S., Moreland, C. J., & Meeks, L. M. (2021). Estimated prevalence of US physicians with disabilities. JAMA Network Open, 4(3). https://doi.org/10.1001/jamanetworkopen.2021.1254
- Moore, S., Kinnear, M., & Freeman, L. (2020). Autistic doctors: Overlooked assets to medicine. The Lancet Psychiatry, 7(4), 306–307. https://doi.org/10.1016/s2215-0366(20)30087-0
- Duong, D., & Vogel, L. (2022). Untapped potential: Embracing neurodiversity in medicine. Canadian Medical Association Journal, 194(27). https://doi.org/10.1503/cmaj.1096006
READ ALSO