Teaching physiology in a participatory and engaging manner to large classes is challenging. The authors take us step-by-step through a simulation-based session on the control of blood pressure for up to 250 students simultaneously: from how to prepare the simulator to how to involve students in interactive simulations to the final assessment.
The most famous prize in our field is given to Physiology or Medicine. There is a good reason for this: with modernity, a deep understanding of physiology became the cornerstone for the practice of medicine. Secondary school students now get a basic introduction to cardiorespiratory anatomy (structure) and physiology (function). This knowledge is deepened for healthcare and bioscience undergraduates as part of their education and training. Most are able to list causes for changes in arterial blood pressure, but how intrinsic reflexes maintain blood pressure on a minute to minute basis is often beyond their grasp. How these responses support blood pressure during stress (e.g. orthostasis) or trauma (e.g. hypovolaemia), and the limits of this feedback control system are rarely well understood. Physiologic model-driven simulation helps learners explore these phenomena in their whole-body and clinical contexts. In this article we tell you about our experience at the University of Bristol.
Target audiences and learning objectives
The learning objective of this class is to explore mechanisms in the regulation of mean arterial pressure by the baroreceptor reflex, and specifically the response to hypovolaemia caused by acute haemorrhage. This facilitator-led class is delivered in Bristol to circa 800 first-year bioscience and healthcare undergraduates in large groups using virtual patients. The same class is used for post-graduate surgical trainees to refresh knowledge of pathophysiology, and for veterinary students, using physiological quantities appropriate for canines.
Before [class design and training media]
The class is structured according to the phases of the hypothetico-deductive method: phenomenon to be highlighted; data gathering; hypothesis formation; prediction; verification; and reflection (Helyer et al., 2024).
A Maestro Evolve simulator (Elevate Healthcare, Sarasota, FL, USA) is used. Clinical signs and monitored signals are automatically generated by a physiological model, responding to removal of increasing volumes of blood. A non-model driven simulator with access to appropriate signs and signals can also be used, but requires scripting of responses, and cannot be made to react to unanticipated interventions suggested by students. It is important to establish the validity of the modelled responses. Minor changes were made to the pre-programmed baroreceptor reflex gain to accurately match the response expected for an 80 kg male patient. Validation was based on data from the scientific literature, both from humans and extrapolated from animals (Lloyd et al,. 2006)
Monitored signals are shown on a clinical monitor emulator and clinical signs can be obtained from a virtual patient. This approach helps students understand the role of monitoring in recognising deteriorating patients. A lead II ECG trace, and systemic arterial and pulmonary arterial and central venous blood pressure tracings are shown on the monitor emulator. A numerical value for peripheral oxygen saturation (SpO2) is displayed, as are values for heart rate (HR), systolic (SYS) and diastolic (DIAS) arterial pressures, and central venous pressure (CVP). Cardiac output (CO) can be shown as a continuous variable, or measured using the thermodilution method. Mean arterial pressure (MAP) can be shown on the monitor or derived from SYS and DIAS. The respiratory rate (RR) is also displayed. Learners derive other quantities using equations provided by the facilitator: stroke volume SV = CO/HR, and total peripheral resistance TPR ≈ MAP/CO. Consciousness can be assessed by the level of alertness of the patient.

To stress the system, a simulated acute blood loss resulting in a BV deficit of 600 ml (10% of total BV) is followed by 3 litres of blood loss (50% of total BV). This is followed by fluid treatment restoring BV to a total deficit of 2 litres (33%), and then to a deficit of 1 litre (17%). Each stage is triggered by the technician advancing the scenario, with clinical signs and monitored signals generated by the model. Learners are guided by a PowerPoint slide set also advanced by the technician. Active learning is promoted by using online polling tools at appropriate times during the simulation, which is also invaluable in assessing progress of learning. Learners enter values in structured data tables.
During (learner activities)
Learners are introduced to the physiological phenomenon. It is explained that the simulated subject was involved in a road traffic accident, but learners are not expected to make a diagnosis or treat them. Need be, time is spent reinforcing knowledge of the mechanism of the baroreceptor reflex and the concept of negative feedback. Data gathering is carried out at every stage.
Phase 0
First the clock is “turned back”, showing monitored variables for the healthy subject during a check-up before the accident took place. This orientates learners to signs and signals to record as the class progresses and reinforces the importance of seeking out healthy baseline values, to be used in later analysis. Hypotheses are formulated for the response to a fall in BV, based on the relationships between BV, CVP & CO, and MAP, CO, & TPR.
Phase 1
This phase represents assessment in the emergency room. The patient is complaining of pain and has lost some blood, revealed to be 600 ml, but is stable. Predictions are made guided by the facilitator, and students note changes in signs and signals, as if observing the trauma progress in real-time. Changes (or not) in HR, CVP, CO and MAP, and derived SV and TPR verify predictions. Learners refine hypotheses on the action of the effector mechanisms that act to restore MAP, ensuring adequate coronary and cerebral perfusion as a priority.
Phase 2
This phase involves a serious deterioration to a total deficit of 3 litres. This illustrates another important clinical point of obtaining repeated and sequential measurements. Predictions are made and verified or falsified by observing changes. To add drama, the monitor emulator alarm sounds, and the patient loses consciousness. Subtle changes are noted on the ECG. Discussion centres on the success, or not, of the reflex in maintaining MAP. Depending on the learner group (scientists or healthcare students), potential treatments restoring BV are discussed. Some invariably suggest administering whole blood, with a useful learning point that normal saline is sufficient to deal with the acute primary problem: hypovolaemia. Observant students report that the value for SpO2 disappears, indicating poor peripheral perfusion and the importance of checking the carotid pulse.
Phase 3
BV is restored in two stages and learners complete the data tables. Blood volumes are not restored completely to pre-accident check-up value, which allows discussion of the concept of permissive hypovolemia that has developed from combat medicine.
After (post-simulation exercises and assessment)
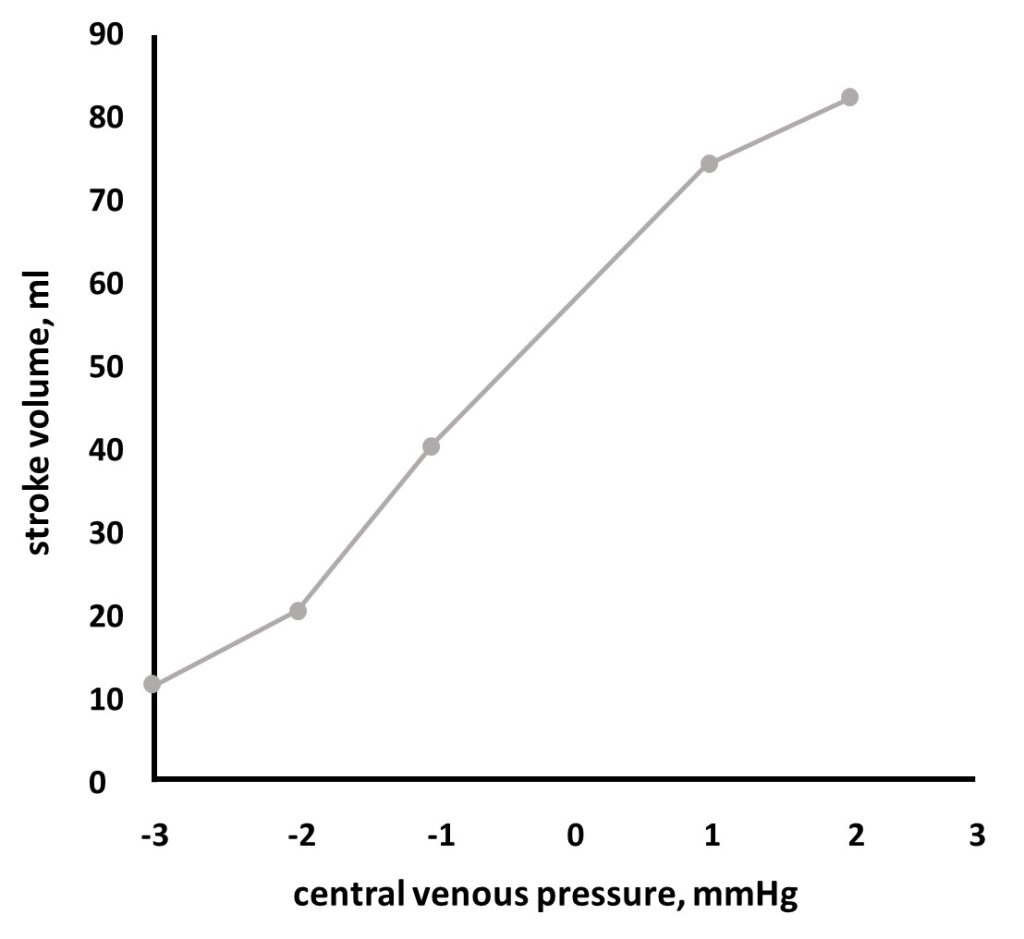
Analysis of data is an integral part of physiology and forms a key part of our approach to teaching physiology. The reflection phase requires learners to analyse, plot, explain data, and draw conclusions based on their observations, predictions, and verifications. These may be carried out in class or as an offline post-class activity. An example is provided in the figure below. Discussed key points include:
- a graph of CVP against SV (or CO). Central venous pressure falls with increasing hypovolemia resulting in a decrease in SV and CO. This relationship leads to the observed effect on heart function explained by the Frank-Starling relationship.
- a graph of the percentage BV deficit against HR, CO and TRP, illustrating compensatory mechanisms of the baroreceptor reflex, and how this mechanism is overwhelmed by very large amounts of blood loss.
- a seemingly paradoxical decline in TPR at the lowest BV illustrates the advanced point of locally mediated factors causing vasodilation, contributing to decompensation as the pre-terminal phase (‘crashing’).
Formative post-class quizzes are used to assess achievement of learning outcomes. Questions based on explanation of mechanisms and handling of data from the simulation are included in summative end-of-module examinations.
In conclusion
This class presents a core physiological phenomenon that cannot (or no longer) be explored on human volunteers or animals. Our experience indicates that this is a highly engaging way of explaining a complex yet clinically highly relevant phenomenon. Learner satisfaction and learner achievement scores are high and match traditional physiology labs, also see (Helyer et al., 2024). Within the limits of available time, the authors can assist colleagues interested in implementing the presented approach.
References
Helyer R, Lloyd E, van Meurs W. Learning Physiology in Context. 112 p. Simedita, Firenze, IT, 2024.
Lloyd E, Helyer R, Dickens P, Harris JR. Human patient simulation in physiology teaching: designing a high fidelity cardiovascular demonstration for first year undergraduates. Proc Physiol Soc. 3: PC62, 2006.
READ ALSO